Electrical Properties of heart:1. Autorhythmicity
The ability to generate action potentials without external stimulus
•spontaneous pre-potential (pacemaker potential) followed by action potential.
•Pacemaker tissue (sino atrial node, atrio ventricular node, atrio ventricular bundle and purkinje fibers) can initiate repetitive action potentials.
•Pacemaker tissue is characterized by unstable resting membrane potential because of its continuous change in membrane permeability.

Pre-potential:
Slow decrease in K+ efflux while permeability of other ions remain constant (through ‘h’ channels and transient ‘T’ Ca2+ channels).
Depolarization:
Ca2+ influx through long lasting Ca2+ channels ( ‘L’ )
Repolarization:
K+ efflux.
Rate of Impulse (per min):
SA node--70-100
AV node--40-60
Atrial and atrial pathway--20-40
Purkinje fibers--20-40
2. Excitability:
Cardiac muscle is excitable tissue
-->it forms a wave of depolarization in response to a stimulus(generation of AP)

0: Rapid depolarization.
Opening of Na+ channels causes increase in Na+ influx.
1: Rapid initial fall in membrane potential (initial rapid repolarization)
Inactivation of Na+ channels.
2: Plateau phase.
Slow opening of Ca2+ channels causes Ca2+ influx.
3: A rapid fall in membrane potential (repolarization phase)
Opening of K+ channels causes rapid K+ efflux.
4: Polarised state.
Ionic composition is restored by activation of Na+K+ATPase pump
3. Conductivity
the ability of cardiac muscle fibers to conduct the cardiac impulses that are initiated in the SA node.
- Impulse from SA node spread quickly to AV node via atrial (internodal) pathway.
- Time delay (0.1 s) occurs as impulses pass through AV node.
- Impulse conduction increases as spread to Purkinje fibers at a velocity of 4 m/s.
- Ventricular contraction begins 0.1-0.2 s after contraction of the atria. (important for ventricular filling phase)
- LBB starts before RBB, as LV wall is thicker so the impulse needs more enough time to reach. Accordingly both ventricles will contract together.
Electrical activity of the heart:
1. Depolarization and origin of cardiac impulse at the SA node. (if SA node doesnt work, AV will take place of being the pacemaker)
2. Conduction of the impulse to all parts of the atria through atrial muscle (there may be some special pathways that conduct impulse fast ie. have a higher conduction velocity). The impulse also spreads to the AV node along the atrial muscle. (Atrial fibrillation occurs when the atrial ms contract independently and continuously bombard AV node with depolarizing waves of varying strength, and depolarization spreads at irregular intervals down the Bundle of His)
3. The impulse will not pass from atrial muscle to ventricles directly as they are not in contact (fibrous tissue separates them). (thus if AV node is blocked, and impulse from SA node couldnt reach ventricle, ventricular muscle will initiate its own impulse as it also has autorhythmicity, eg. seen as AV dissociation on ECG)
4. AV node has a low conduction velocity and thus the impulse takes sometime to travel across it. It eventually travels across it and reaches the upper end of the bundle of His.
5. Bundle of His has a high conduction velocity. It conducts the impulse through its branches to the Purkinje fibre network just under the endocardium of the ventricles. (In a normal conditionn where impulse is able to be transmitted from AV node to Bundle of His, impulse created by ventricular muscle itself doesnt cause muscle contraction as the impulse hits the absolute refractory period--all/none law of the action potential of cardiac muscle that is stimulated by normal conduction system's impulse)
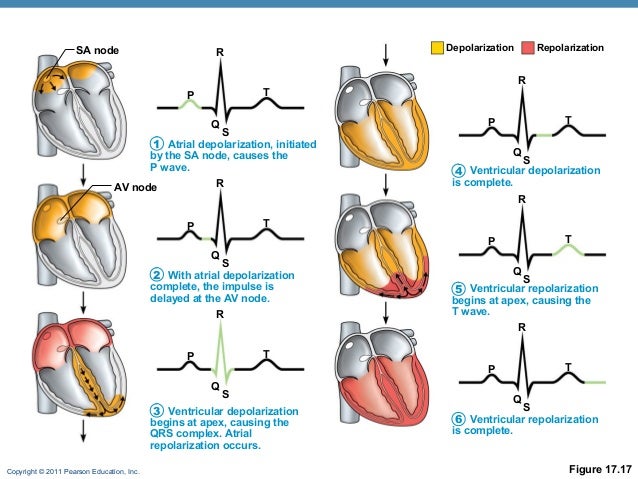
*atrial repolarization not seen on ECG as it was masked by the stronger ventricle depolarization
******************************************************
Mechanical Properties of the heart:1. Contractility
---when an action potential occurs in the muscle it responds by contraction.
During excitation-contraction coupling the ER releases some Ca++ ,but to have sufficient calcium for contraction there must be influx through the sarcolemma. Hence the importance of the plateau phase of the action potential.
- For cardiac muscle, the amount of stretch of the muscle before a contraction has special significance and is called preload (Starling Law).
- Protected from tetanus because of its long ARP
- No recruitment of cardiac muscle fibers.
- Strength of contraction of cardiac muscle depends to a great extent on the concentration of calcium ions in the ECF
- Action potential of cardiac muscle is an all or none law response to a stimulus.
- If the stimulus is sub-threshold (inadequate), no action potential is produced.
- If the stimulus reaches threshold, a full-fledged action potential is produced.
- Further increase in the intensity of a stimulus produces no increment in the amplitude of AP.
Absolute refractory period:
- The excitability of cardiac muscle is completely lost during this period, i.e. doesn’t respond to 2nd stimulus.
- Occupies the whole period of systole.
- The excitability of cardiac muscle is partially recovered during this period, i.e. stronger stimuli than normal are required to excite the muscle.
- Occupies the time of diastole.
- Can be affected by the heart rate, temperature, vagal stimulation, sympathetic stimulation & drugs.
******************************************************
Factors affecting heart rate:
Factors affecting heart rate:
1. Sympathetic stimulation
Act via β1-adrenergic receptors -->increase cAMP-->Increases heart rate by opening of Ca2+ channels--> increase Ca2+ influx-->increase rapidity of the depolarization phase--> increase heart rate (positive ‘chronotropic’ effect)
2. Vagal stimulation
Acts via M2 muscarinic receptors -->decreasing cAMP-->Decreases heart rate by opening of K+ channels and slows the opening of Ca2+ channels --> increase K+ efflux of nodal tissues -->hyperpolarization --> decrease slope of pre-potentialp--> decrease firing rate--> decrease heart rate (negative ‘chronotropic’ effect)
3. Temperature
Arise in body temperature by 1 °C increases the heat rate by 10 beats/minute.
The rise in body temperature increase the heart rate by increasing the permeability of the membrane to Ca++ during the pacemaker potential.
4. Sinus arrhythmia
Variation in R-R interval during deep inspiration.
During deep inspiration, lung stretch--> inhibits cardio-inhibitory center-->decreases tonic vagal discharge -->increases HR.
5. Ion concentration in ECF
K +
-the early effect of mild hyperkalemia on myocyte function is to increase myocyte excitability by shifting the resting membrane potential to a less negative value and thus closer to threshold potential; but as potassium levels continue to rise, myocyte depression occurs and Vmax continues to decrease.
A plasma potassium of >6.5mmol/L (normal 3.5-5.5) is an emergency, myocardial hyperexcitability--> ventricular fibrillation--> cardiac arrest
5.5-6.0 mEq/L - Mild
6.1-7.0 mEq/L - Moderate
7.0 mEq/L and greater - Severe
Sx: fast irregular pulse, chest pain, weakness, palpitation, and light-headedness
ECG: Tall tented T wave, small p wave, wide QRS complex

Causes:
Decreased or impaired potassium excretion - As observed with acute or chronic renal failure (most common), potassium-sparing diuretics, urinary obstruction, sickle cell disease, Addison disease, and systemic lupus erythematosus (SLE)
Additions of potassium into extracellular space - As observed with potassium supplements (eg, PO/IV potassium, salt substitutes), rhabdomyolysis, and hemolysis (eg, blood transfusions, burns, tumor lysis)
Transmembrane shifts (ie, shifting potassium from the intracellular to extracellular space) - As observed with acidosis and medication effects (eg, acute digitalis toxicity, beta-blockers, succinylcholine)
Fictitious or pseudohyperkalemia - As observed with improper blood collection (eg, ischemic blood draw from venipuncture technique), laboratory error, leukocytosis, and thrombocytosis
Management:
Urgent:
- Stabilize Cardiac membrane with 10ml 10% calcium gluconate
- drive K+ into cell with 10 units actrapid in 50ml 20% glucose
Non-urgent: (K+ not >6.5, no myocardial hyperexcitability)
- Treat underlying causes.
- Polystyrene sulfonate resin 15g/8h PO
Ca2+ ion in ECF
- Increase in Ca2+ concentration --> increase cardiac contractility
- Decrease in Ca2+ concentration --> decrease cardiac contractility
6. Blood flow
Insufficient blood flow--> decreased oxygen and nutrient supply--> decreased heart conductivity and metabolism
7. Drug
Sympathomimetic drug--> increased HR
parasympathomimetic drug--> reduce HR