HISTORY
Patient
identification
1. Name
2. Age
3. Ethnic
4. Lady
5. Occupation
6. Address
7. Date
of admission and clerking
8. Informant
9. Gravida
- No. of pregnancy irrespective of the outcome
10. Para
- No. of delivery
of ≥ 24 wks of gestation / > 500g (including stillbirth)
- Twins
are counted as 2
e.g: never pregnant before G1P0. If
she delivered twins & come back next time at
12 wks, she will be G2P2 (twin)
- If
abortion (delivery < 24 weeks / < 500g), put ‘+ number of
abortion’
e.g: If abortion for 2 times and now she
pregnant, she will be G3P0+2
*miscarriage occurred by accident, abortion occurred
by planned surgery
11. Last menstrual period (LMP)
- 1st
day of last menses (ask hari pertama tak boleh sembayang)
- LMP
reliable must fulfil Naegele’s rule:
* Sure of date
* Regular menstrual
cycle 28-30 days
* Not on breastfeeding within 2 mths
(If
exclusively breastfeed, ovulation will not start in 1st 3rd
month; if not
exclusively,
ovulation will occur at the 3rd month)
* Not on
hormonal therapy within 3 mths
(mention the Naegele’s rule in history to
see one is fulfill
- If LMP
not reliable:
* Ask about early U/S (<20w)
# 1st trimester: difference 1 wk;
2nd trimester: difference
2 wk
3rd trimester:
difference 3 wk
# If the scan date is corresponding to the EDD, use EDD
# If not corresponding, use the rEDD
# POA that is counted from rEDD should be presented as POG (period of gestation)
Mention date for each U/S
For U/S 1st trimester is the most accurate
reading the discrepancy of rEDD compared to real date of delivery is 1 week.
For 2nd trimester is 2 weeks discrepancy.
For 3rd trimester is 3 weeks.
12.
Other ways for dating:
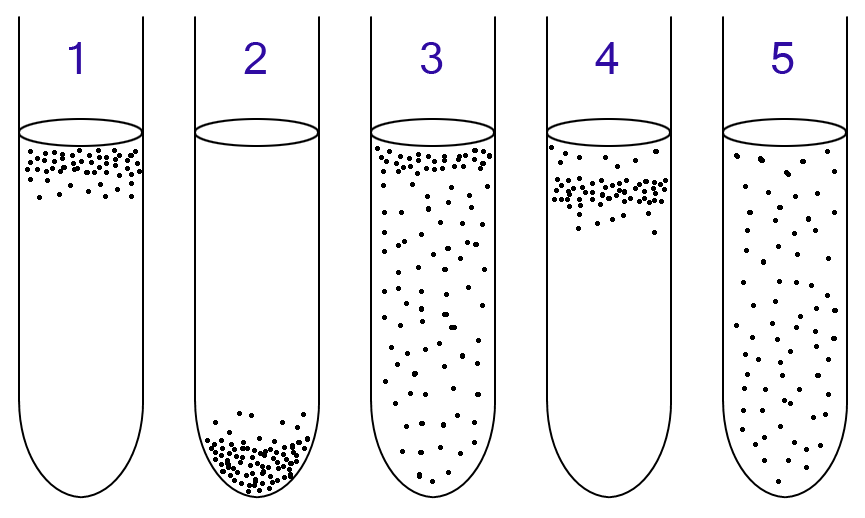
- UPT in dilution (1st
positive 6-8wk)
- quickening
- uterine size corresponding to date
- histopathology (presence of
chorionic villi- either passed out
spontaneously or from curettage
specimen)
|
|
Expected date of delivery (EDD)
- LMP + (9 moths 7days)
13. Periods of amenorrhea (POA)
- counted from LMP to date of clerking
- present as ?weeks ?days
1 month= 4w + 2 days
2 months= 8w+ 5 days
3 months= 13w
(prof adibah: every 3mth- add 1 week (3x4+1=13))
Comment:
The LMP is ___. It fulfils the Naegele’s
rule. U/s was done at___ weeks which is corresponds to the EDD, therefore the
EDD is___/ not correspond to EDD, therefore, the rEDD is___
* u/s scan: normal EFW
- 24 wk: <1kg
- 28 wk: 1.4-1.8kg
- 32 wk: 2kg
- 36 wk: 2.4kg
* normal weight gain:
- 1st 5mths: 0.5kg/mth
- 2nd 5 mths: 0.5kg/wk
Chief complaint
- Complaint + duration
History of presenting illness (HOPI)
- ask about chief complaint or any related question (associated sx/ risk factors/ cx)
- at the end of HOPI, ask about:
* is patient in labour ?
# contraction pain (how many times in 10mins? each
contraction last for how long?
regular?
↑ frequency and intensity?)
# show- blood stained mucus passed PV
# leaking liquor
* fetal movement (good or ↓?)
(ask
the patient to count how long for fetal kicks for 10x, look for the pattern of time
completion- see the FKC)
FKC is a chart given at 3rd
trimester. Counted everyday from 9am-9pm. 1 KICK= 1 kick, or multiple kicks at
one time, or 1 rolling. When mother sensed there are 10 kicks in total, she
will made a tick at the time of completion of 10kicks(eg. Usually 1pm) at the
chart. Another version is fast Fetal Kick Chart which only required counting 10
kicks in 2 hours, for busy mother. If kicks is less than 10 in a day(from
9am-9pm) indicative of reduced fetal movement.
London used Cardiff county method.
Fetal movement reduced, possible causes:
1.
Mother is fatigue, (involved in strenuous activity),
less energy provided to baby
2.
Infection, if mother is having fever, fetal
temperature is 1 degree Celsius more than the mother
3.
Trauma, in kampong, mother rode motorcycle
or multigravida mother, the abdomen was kicked by her naughty children in fight
4.
Mother took sedatives
5.
Mother is malnourished, can be due to
taboo(wrong thoughts about some food could cause harm to baby), nausea and vomiting(cannot
eat much)
6.
Mother went for lenggang perut, reposition
of baby by traditional healer causing cord around neck
7.
Baby is hypoxic, placenta insufficiency
8.
Increased in amniotic fluid or uterine
contraction (cannot sense the kicks)
9.
Sometimes can be just due to mother too busy
and not correctly count or too worried as she had experienced miscarriage or similar
experience in previous pregnancy
10. IUD is usually dued to abruption placenta, no kick at
all.
Hx should mention –ve trauma, -ve sx of
infection(eg. UTI sx), -ve goin to traditional healer, and diet balance.
**no need systemic review if all +ve n –ve sx
had been illicited
- briefly about what is done in hospital
|
|
Comment:
She missed the
period for __weeks. She did the UPT and was found to be +ve
|
|
Systemic review
History of presented pregnancy
Present HOPP in sequence, 1st, 2nd,
then 3rd trimester
- suspect pregnancy
* why- missed
period? Quickening? Abdominal distension?
* when?
Missed period state when, at 6th week since
last period? Did she do UPT herself? When UPT is +ve, did she go to the clinic
immediately, if no state why?
*UPT can only be positive at 2 w after ovulation which
means 1 mth after the last period
- confirm pregnancy
* when? where?
who?
* u/s?
Which clinic?
- booking= 1st antenatal check-up
* when? where?
(bila ambil kad merah?)
* physical
examination
ANC:
- Monthly till 28
weeks
- Fortnightly
till 36 weeks
- Weekly till
delivery
|
|
# height,
weight, BP, fundal height
* investigations
# blood
test- blood group, rhesus, Hb
Comment:
- blood and urine
test were done
and were normal
- screening test
were not reactive
- mOGTT was done at
__wk with
reading __/__
- BP, height and
weight were
normal
- For the
subsequent ANC, u/s
scan and fundal assessment
show fetal growth correspond to
gestational age and amniotic
fluid is adequate, no congenital
abnormality detected
|
|
# Urine test- glucose, protein
# VDRL
(reactive/non-reactive), HIV
- mOGTT done? Indication? When? Result?
- subsequent antennal check-up
* when-
patient attend all ANC follow schedule?
* parameter-
normal?
* weight gain
* BP
* Uterine size
* Hb
* Urine
glucose and protein
* U/S done?
- When?
- Any
abnormalities
Things to be stated from booking: Height, weight, bp,
urine protein n glucose, hb, blood group, rhesus, VDRL, Hep B, HIV
(try use clerkin in osce/long case, ask the patient
whether she remembered the parameters instead of copy from the redbook, if she
cant remember, ask if doc comment anythg, any abnormalities)
Antenatal checkup is done every 4w in 1st
tri, every 2 w in 2nd tri and every week in 3rd tri
10-12w
: correct dating (dating scan)
20-22w : to detect any congenital abnormality
28w : to detect location of placenta
32w : to final confirm the location of placenta
|
|
Quickening:
- Primigravida=
18-20w (5 months)
- Multigravida=
16-18w (4 months)
|
|
- Quickening- 1st fetal movement
* When?- bila berasa bayi pertama kali
bergerak?
* ↑ intensity
and frequency?
- Signs and symptoms of pregnancy
* nausea and
vomiting
* breast
discomfort/engorgement
* frequency of
urination
* constipation
* ankle edema
* backache
- immunization:
* anti-tetanus
toxoid (ATT) - IM 0.5mL
# Primigravida
- 1st
dose after quickening (20-24w)
- 2nd
dose - 4-6 weeks after 1st dose (24-28w)
-
latest 4 wks before delivery
# Multigravida
- One dose only after quickening (usually at 32-36w)
* Hepatitis B
(3X)
* Rubella
(usually during school times)
Past obstetric history (POH) – no need present if
primigravida- only marital status
- Marital status
* When
married?
* Married at
age?
* 1st
married? the only married? (related with pregnancy
induced hypertension)
* Consanguineous married? (related with chance of genetic disease transmission)
- no of children? How many boy and girl?
- for each pregnancy:
* age
* sex
* where
deliver- hospital? Clinic?
* when- full
term? POG if preterm?
* method of
delivery
# spontaneous
vaginal delivery
# induced
vaginal delivery: Postdate, PIH, GDM, heart disease etc
# assisted
vaginal delivery- forceps? Vacuum? Why? Prolonged labour, heart dz etc
# lower
segment caesarean section- elective/emergency?
(a) why? where? POG?
(b) duration of staying in wad- 5 days if no Cx
(c) cx- PPH, blood transfusion,
fever, scar pain
(d) any VBAC
after the caesarean section?
* ask the
indication except SVD
* birth weight
# low birth
weight < 2.5kg
if all deliveries are normal, summarize ‘no
AP,IP,PP Cx’ at the end of presentation of POH
|
|
# big baby > 4.0kg
* antepartum
Cx- APH, placenta praevia,
* intrapartum
Cx- poor progress, fetal distress
* postpartum Cx- PPH, lochia changes, fever
* breastfed
till when?
# normally for
2 yrs (exclusive 6 months)
# if stop
early/bottled feeding-why?
- if abortion
* POG?
* why?-
spontaneous? Trauma?
* signs and
symptoms before abortion.
* dilatation
and curettage (D&C) done?
# D&C- incomplete abortion
# no D&C- complete abortion
- if >5 children
* Summarize
all the uneventful deliveries (FTSVD with no Cx)
* eldest what
age? youngest what age? birth spacing?
* all born
through FTSVD with no AP, IP, PP Cx
* BW range
* breastfeeding
* developmental
growth
* Mention the
abnormal deliveries separately
- spacing
* good spacing-
2 years apart
* abnormal->
6 years, why? contraception? Subfertility?
- contraceptive method:
* OCP/
injection/ implantation
* IUCD
* condom
For complication of C-sec,
1. Anesthesia, half or full
2. Bleeding? Any blood transfusion
3. Injury to organ, bladder? Rectum?
4. Post-op, well?
Csec: indication to do, complication, venue which
hospital
Past Gynaecology History (*combined together and state
gynae hx)
- menstrual
history
* when attain
menarche (1st menstrual period)? Normal 9-16 y/o
* menstrual
cycle
Written as:
Age of menarche flow
cycle
|
|
# regular/irregular
# cycle-
normal 21-35 days
# flow-
normal 2-8 days
# heavy
flow- normal 1st-3rd day
# pad
used-average blood loss 30ml
# problems
(a) dysmenorrhoea- painful
menstruation
(b) menorrhagia- prolonged and
increased menstrual flow (blood loss>80ml)
(c) intermentrual bleeding
(d) postcoital bleeding
(e) dyspareunia- painful coital
- pap smear history
* how many
times?
* when was the
last one?
* result
normal?
Past medical and surgical history
- hx of chronic illnesses: HPT, DM, heart disease,
asthma, TB
- any surgery procedure done before?
Family history
- siblings and parents- health problem
- family hx of HPT, DM
- Family hx of twins preg or congenital abnormality
Personal and social history
- education level
- husband’s age, occupation (type, work place, daily
come back), income
- house condition: stair, toilet and etc
- how frequent husband visit her?
- who take care of her children during admission?
- how does she contact her children?
- smoking? alcohol?- both husband and pt
Transportation at home, some pregnant lady ride
motorcycle
Nearest clinic from home? Convenient to checkup?
Drug history
- hematinics
* iron- besi
(T. ferrous fumarate 200mg contain 60mg iron)
* folate- ubat
kuning kecil (5mg/tablet)
* vitamin B12
&C
- over counter drugs: Obimin (contain iron, folate,
Vit B12 and etc)
- traditional medication
- allergy/ side effect
Obimin contained all four, iron(ferrous fumarate,
folic acid, B12 and Vit C)
Obical include obimin plus calcium
The all four are enough for what required for mother
Dietary history
- normal balance adult diet
- allergy
- if patient is diabetic, details diet history are
needed, including dishes for every meals,
who give the
advice? was pt understand, give eg of food?
Summary
Name/ age/ race/ gravida/ para/ POA/ chief
complaint/ complication/risk factor/ management that been given/ in labour or
not/ fetal movement
lightening: primigravida at 34 wk when head enter the pelvic brim (mother will
felt sudden relief of SOB or breathing discomfort)
PHYSICAL
EXAMINATION
Before start
- introduce pt to dr
- introduce dr to pt
- ask permission from pt and ask for chaperone
- position: Lying flat
- pt comfortable? With both
hands at the side of body
- pt can sit upright if she had sign of cardiac
disease or grossly enlarged uterus (cause
splitting of
diaphragm)
General examination
- Inspection:
v Comfortable, lying flat/ propped up supported with one pillow
v Alert and conscious
v Well orientated to time, place and person
v In pain, in respiratory distress
v Hydrational and nutritional status
v Gross deformity
v Abnormal movement
v Attachment
v Height : <148cm and small shoe size→ smaller pelvic capacity→ CPD
v Weight
v Hand:
·
Warm/cold, dry/sweat
·
* Mother with HPT is not advice to wear
ring (edema)
|
|
Pale
·
Palmar erythema (↑ estrogen level)
·
Koilonychias (iron deficiency)
·
Peripheral cyanosis
·
Clubbing
·
Capillary refilling
·
Collapsing pulse (pathological/physiological d/t
hyperdynamic circulation)
v Vital sign:
·
Pulse rate, volume and rhythm
·
BP (sitting position or prop up 45 degree) pregnancy
induced HPT dx after 20 w with measurement of high bp in 2 occasions
·
RR
·
Temperature
v Neck:
·
JVP- if indicated
·
Thyroid swelling (normal for pregnant mother as they
usually experience iodine deficiency)
v Face and eyes:
·
Jaundice in sclera
·
Pallor on conjunctiva
·
Mouth, lips and tongue:
- Tongue: Moist/ Coated
- Oral hygiene
- Central cyanosis
- Glossitis- nutritional
deficiency
- Angular stomatitis-
nutritional deficiency
- Oral thrust- candidiasis
v Leg:
·
Pitting edema
·
Dilated vein
v Examine reflex and fundoscopy for hypertensive patient
Specific examination
(a) Before
start:
v Ask permission
v Exposure- xyphisternum to symphysis pubic
(not nipple line to mid-thigh!)
Prof Nora- expose from lower border of bra
to pubic symphysis (ask chaperone or examiner to expose the patient)
(b) Inspection:
v Abdomen is distended with gravid uterus evidenced by
·
Linea nigra
·
Striae
gravidarum-red, present stretch mark
·
Visible fetal movement
(Prof Nora- show the findings by pointing it
with thumb)
v Striae albicans- white, previous stretch mark
v Move symmetrically with respiration
v Umbilical: Centrally located and Inverted/flat/everted
v Dilated vein
v Surgical scar
·
Laparoscopy: Umbilical; Small, easy to miss
·
LSCS: Transverse suprapubic/ pfennential scar
·
Upper segment caesarean section: Paramedian
* If there
is scar
-
site, size, shape
-
well heal/infected/keloid
-
surrounding skin- pigmentation, redness, swelling, ulceration, discharge
- look for scar tenderness during
palpation. (palpate around the scar to look for
uterus tenderness)
v Inguinal cough impulse
(c) Palpation:
(examiner sit down n patient lie flat!!!!)
v Superficial palpation: Soft, tenderness
(comment-
the abdomen is soft and not tender)
v Deep palpation: Contractile uterus
(comment-
the uterus is soft, not tender and not irritable)
(if
present of contraction- palpate at the fundus and time the contraction)
(don’t
perform deep palpation for Prof Nik Haslina)
v Fundal height
·
Symphysiofundal height
- Palpate the fundus using ulnar border of left hand from xiphisternum
12w- just above suprapubic
22w- umbilicus
36w- xyphisternum
|
|
- Put the tape with inch scale on top
- Palpate for symphysis pubic (midline, 1st bony prominent)
- Measures in cm (1w= 1cm)
·
Clinical fundal height (some dr no need present this…)
- Estimate how many finger breadth the fundal palpable below
xyphisternum/above
umbilical
(don’t use
finger to count- Prof Nik Haslina)
- Count fundal height (1w=1cm)
* After
36w- below xyphisternum (less 1cm for every week) but there is fullness of
flank
and cannot get below the costal margin)
* Mention
as ‘’fundal height is __ weight’’
* Fundal
height corresponding to POA?- allow +/- 2cm
Example 1: pt in 38w POA
The symphysiofundal height was 33cm. The fundus was palpable one finger breath
below xyphisternum. There was fullness of flank and I could not get below the
costal margin. The clinical fundal height was 38w which was corresponding to
the POA.
Example 2: pt is in 34w POA
The symphysiofundal height was 34cm. The fundus was palpable 1 finger breath
below xiphisternum. There was no fullness of flank and I was able to get below the
costal margin. The clinical fundal height was 34w which was corresponding to
the POA.
Notes:
- symphysiofundal height is not very reliable in
assessing the uterus size if you only see your patient for the 1st
time because it is influenced by other
factors, e.g. obese and thin, amount of amniotic fluid,
fetal weight.
- symphysiofundal height is useful when you f/u the
patient during antenatal visit. You can assess the ↑ in symphysiofundal height
compared to last visit.
Pawlick grip:
- can not performed by medical student
- using thumb and pointing finger to grip at
the fetal head
|
|
(d) Grips (Leopard’s)
- Fundal grip
·
face patient
·
feel the fundus using both hand
- lateral grip
·
face patient
·
* causes of head not engaged:
- placenta praevia
- polyhydramnios
- pelvic mass/ uterus mass (fibroid)
- CPD
|
|
fix one hand and palpate with another hand
- pelvic grip
·
face patient’s leg
·
feel with both hands
·
feel for engagement
- comment on:
- singleton/ twins
- Lie- relation of long axis of fetus to the long axis
of uterus
* longitudinal
(normal), transverse, oblique
- Presentation- pole of fetus that presents on pelvic
brim
* cephalic
(normal), breech
- Engagement (for cephalic presenting)- the largest
presenting part enter the pelvic brim
·
If ballotable= not engaged
·
use 5 fingers to measure
·
if 3 fingers palpable per abdomen= 3/5th
palpable
·
2/5th palpable per abdomen= engaged
-
liquor volume- clinically adequate?
-
fluid thrill if excessive liquor
-
estimated fetal weight
Polyhydramnio: when palpate hand need to go deep more
than 8cm to feel fetal
Oligo: hand less than 2cam
·
Head- round, hard,
ballotable
·
Buttock- broad, firm, not
ballotable
·
Fetal back- smooth, firm,
continuous
·
Fetal parts- bulging
·
Excessive liquor (large
fundus, can’t feel fetal parts, + fluid thrill)
·
Reduced liquor (tense
abdomen, easy to feel fetal parts, small fundus)
|
|
Reason oligo: HPT, placenta insufficient
(e) Auscultation:
·
For fetal heart sound-present/ not present
·
Use pinard (don’t stress on look at patient face,as
long as
·
Comfortable n hands off pinard)
·
Listen at anterior shoulder
·
Dont press too hard and both hands off when listen!!
·
Must count HR (normal 120-160)
(f) Complete examination with:
·
Per vaginal examination (C/I-
in PV bleeding/ leaking liquor)
·
Breast examination: important
for breastfeeding
·
l/n examination
·
Others systems if relevant
Present:
- From inspection, the abdomen was
distended with gravid uterus evidenced by presence of linea nigra, striae
gravidarum, visible dilated vein and fetal movement. There were __ striae albican and ___ scar (type, length,
well healed/not, sign of inflammation, tenderness). The umbilicus is centrally
located and ___
- On superficial palpation, the abdomen is
soft and not tender.
- On deep palpation, the uterus is soft,
not tender and not irritable.
- The SFH was ___ cm correspond to POA/POG.
The fundus is palpable __FB below xiphesternum. __ fullness of flank and ___
get below costal margin. The clinical fundus height is ___wk
- There is ___ fetus with ___ presentation,
___ lie. The fetal back is at maternal __side and fetal part at maternal __
side. Fetal head is __/5th palpable, __ engaged. Fetal movement __
felt and __ uterus contraction. Liquor is clinically __. FW is __kg (range with
interval 0.2)
- Fetal heart was heard at __ quadrant
using Pinard and heart rate is __ bpm
# Prof Adibah: evidence of gravid unterus: only fetal movement and fetal heart
Investigate
U/S
: check anencephaly, cord around neck, growth restriction
CTG: Fetal distress: check whether HR normal, whether
there is acceleration (normal)
Urine FEME: check UTI
FBC: ANEMIA, INFECTION
Placenta blood flow, check using doppler ultrasound,
Normal position of placenta, upper segment
Mx for reduced fetal mov:
Admission, bedrest, fetal kick chart, CTG daily