Normal Venous Circulation in Leg
Two venous systems are found in the lower extremity, the deep and superficial, as depicted in the image below. The deep system ultimately leads backs to the inferior vena cava, then to the heart. The superficial system is found above the deep fascia of the lower extremity, within the subcutaneous tissue. Many superficial veins exist, but they all drain into the 2 largest superficial veins, the greater saphenous vein (GSV) and the short saphenous vein (SSV), formerly called the lesser saphenous vein.
The superficial venous system is connected to the deep system at a number of the following locations:
- Perforator veins: These veins traverse the deep fascia of the lower extremity. A number of named perforators are found at the thigh, knee, and leg.

- Saphenofemoral junction (SFJ): This is located proximally at the groin where the GSV meets the femoral vein, as depicted in the images below.


- Saphenopopliteal junction (SPJ): This is located behind the knee where the SSV joins with the popliteal vein.
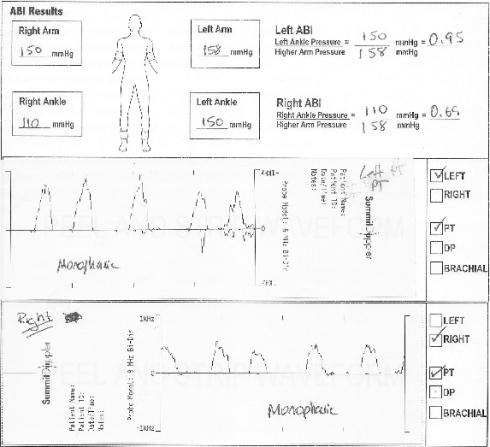
In healthy veins, the flow of venous blood is through the superficial system into the deep and up the leg and toward the heart. One-way venous valves are found in both systems and the perforating veins. Incompetence in any of these valves can lead to a disruption in the unidirectional flow of blood toward the heart. In 53% of patients only superficial venous reflux was found, in 15% isolated deep venous reflux was found, and in 32% a combination of deep and superficial venous reflux was found.
Incompetence in the superficial venous system alone usually results from failure at valves located at the SFJ and SPJ. The gravitational weight of the column of blood along the length of the vein creates hydrostatic pressure, which is worse at the more distal aspect of the length of vein.
Incompetence of the perforating veins leads to hydrodynamic pressure. The calf pump mechanism helps to empty the deep venous system, but if perforating vein valves fail, then the pressure generated in the deep venous system by the calf pump mechanism are transmitted into the superficial system via the incompetent perforating veins.

Once venous hypertension is present, the venous dysfunction continues to worsen through a vicious cycle. Pooled blood and venous hypertension leads to venous dilatation, which then causes greater valvular insufficiency. Over time, with more local dilatation, other adjacent valves sequentially fail, and after a series of valves has failed, the entire superficial venous system is incompetent.

The clinical finding of varicose veins, reticular veins, and telangiectasia are due to the hypertension in the superficial venous system that spreads to collateral veins and tributary veins.
In contrast to the superficial veins, the deep veins do not become excessively distended. They can withstand the increased pressure because of their construction and the confining fascia.
Examination of Varicose Vein
Perthes maneuver/Linton test: This is a physical examination technique in which a tourniquet is placed over the proximal part of the leg to compress any superficial varicose veins while leaving deep veins unaffected. The patient walks or performs toe-stands to activate the calf-muscle pump which normally causes varicose veins to be emptied. However, if obstruction of the deep system exists, then activation of the calf-muscle pump causes a paradoxical congestion of the superficial venous system and engorgement of varicose veins resulting in a positive test. To verify, the patient is then placed supine, and the leg is then elevated (Linton test). If varices distal to the tourniquet fail to drain after a few seconds, again deep venous obstruction must be considered.
Once the dilated veins of the leg are marked, the Brodie-Trendelenburg test can be performed. With the patient in the supine position and the leg elevated 60°, emptying the varices of blood by stroking distally to proximally is performed, and a tourniquet is placed around the proximal thigh. The patient then stands up, and the leg is observed for 30 s with the tourniquet in place. The following responses can be seen:

- “Nil” test: (Competent valves of the deep and perforating veins and at the saphenofemoral junction): No distention of the veins for 30 s both with the tourniquet in place and after removal
- “Positive” test: (Incompetent valve at the saphenofemoral junction): Distention of the veins only after release of the tourniquet
- “Double” positive test: (Incompetent deep and perforating veins, with reflux through the saphenofemoral junction): Distention of veins with the tourniquet in place and further distention after release
- “Negative” test: (Deep and perforating valvular insufficiency): Distention of veins within 30 s of the tourniquet in place, and no increased filling after release of the tourniquet. However, filling of the vein(s) after 30 s of tourniquet placement does not imply competence of perforating veins.
The percussion/Schwartz test is performed by placing one hand over the saphenofemoral junction or the saphenopopliteal junction while the other hand is used to tap lightly on a distal portion of the long or short saphenous vein. The presence of an impulse implies valvular insufficiency in the segment between the two hands.

Morrisey’s Cough Impulse test
- Ask patient to stand.
- Use finger to held over patient's saphenofemoral opening [5cm below and medial to femoral pulse].
- Ask patient to cough.
- If saphenofemoral junction is incompetent, there is presence of fluid thrill.
Fegan’s test

Pratt test
The Pratt Test is a simple test to check for Deep Vein Thrombosis in the leg. It involves having the patient lie supine with the leg bent at the knee, grasping the calf with both hands and pressing on the popliteal vein in the proximal calf. If the patient feels pain, it is a sign that a DVT exists.
Multiple Tourniquet Test

*Do not confuse Trendelenburg Test with Multiple Tourniquet Test
Trendelenburg test is to apply one tourniquet below (for example SFJ). If during the tourniquet is applied, there is filling of varicose vein(which you had just emptied before the test), it means the pt’s perforating vein is incompetent, blood flow from deep vein to superficial vein. If after applied, no filling, and when you release the tourniquet and there is filling, it means the SFJ above your tourniquet is incompetent and cause downward flow of blood because of the gravity. However,For multiple tourniquet test, it is simply used to test perforating veins, so don’t think about the superficial vein. Multiple tourniquets are applied to occlude the superficial vein at different area. For example one at the mid thigh and one above the knee. So normally when without tourniquet, if blood flow from the incompetent perforating vein to superficial vein, it might flow downward when it’s in the superficial vein(if there is further incompetent valve), or it will be carried upward to the SFJ and so on…
So applying tourniquet is to occlude the superficial vein above and below the area which the perforator vein has problem. So that we can see the pooling of blood at the varicose vein there(remember that you already empty the varicose vein before the test by elevate leg and also rub the veins).
So for multiple tourniquet, the result is not to be acquired by releasing the tourniquet, but is during which the tourniquets are applied. So, for my personal opinion, it doesn’t matter whether you remove them from bottom to above or from above to bottom.
The purpose of doing all these tests is to determine the area so as to perform surgery on the problem veins. But these tests are not so important nowadays provided that technology such as colour flow imaging, magnetic resonance venography can already help to give a better image. Varicose veins can cause complications such as ulcers beside just comestically undesirable. So, sometimes surgery to take out the varicose vein is necessary. However, nowadays, other methods such as sclerotherapy is also used.
Adapted from: Medscape and Some old surgery books